Addition of a Sagittal Cervical Posture Corrective Orthotic Device to a Multimodal Rehabilitation Program Improves Short- and Long-Term Outcomes in Patients with Discogenic Cervical Radiculopathy
Purpose of the study
Investigated whether adding a posture-correcting orthotic (Denneroll) to an existing multi-component rehab program improves pain, function, and nerve function in patients with discogenic cervical radiculopathy (DCR)—a condition where disc problems cause nerve root compression in the neck.
Study Design
Type: Randomized Controlled Trial
Participants: 60 patients with chronic DCR, reduced cervical lordosis (loss of natural neck curve), and forward head posture
Intervention group: 30 patients (mean age ~41.5 years)
Control group: 30 patients (mean age ~43.9 years)
Interventions
Both groups received a multimodal rehabilitation program, including:
Manual therapies (e.g., spinal manipulation, stretching, myofascial release)
Physical modalities (TENS, heat)
Functional exercises for posture, strength, flexibility
Home-care instructions
Intervention group additionally used the Denneroll cervical orthotic device—a posture correction orthotic designed to improve cervical lordosis.
Outcomes Measured
Cervical lordosis (curve angle)
Anterior head translation (AHT)
Pain: neck & arm
Disability: Neck Disability Index (NDI)
Nerve function: Dermatomal Somatosensory Evoked Potentials (DSSEPs) and central conduction time (N13–N20)
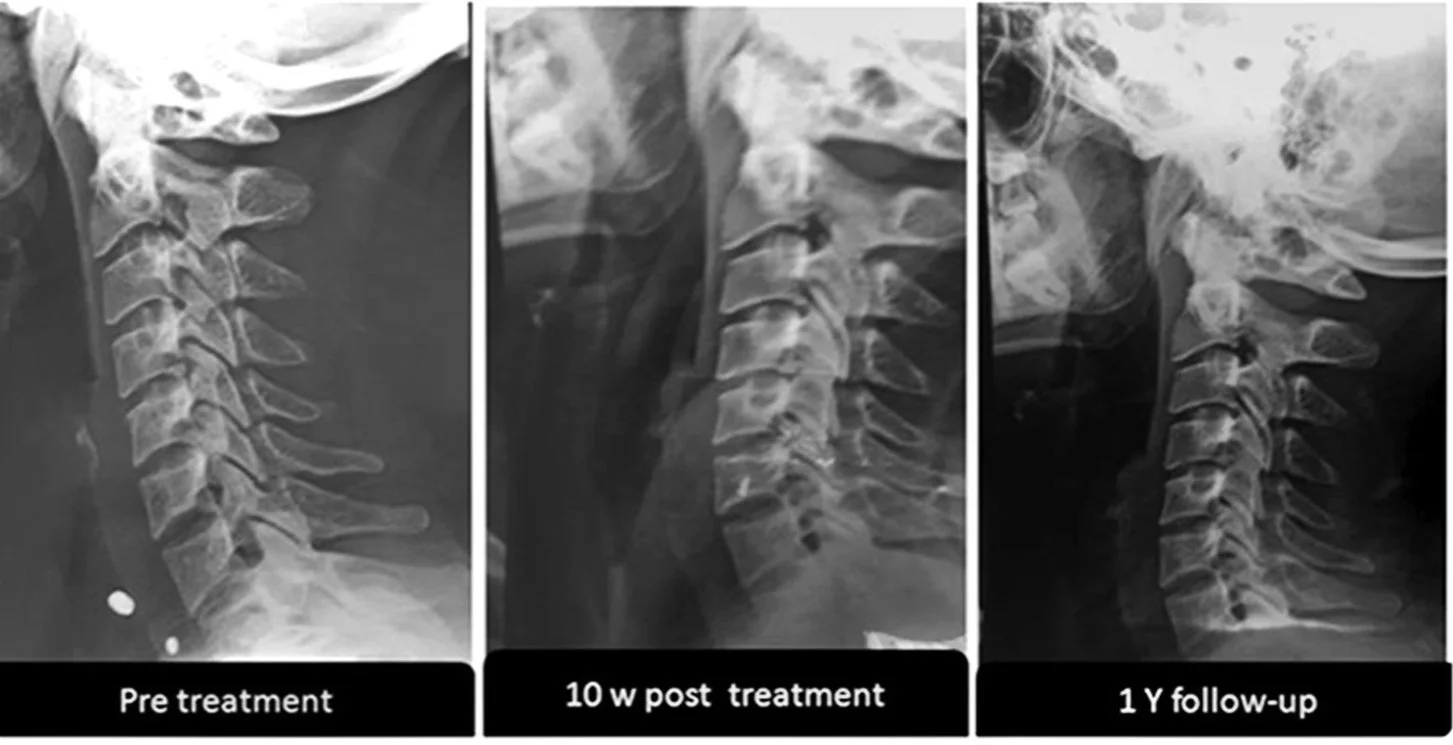
Evaluated at baseline, 10 weeks, and 1 year
Results
At 10 weeks:
Both groups had similar arm pain, neck pain, and DSSEP latency improvements.
Intervention group had significantly better outcomes in:
Cervical lordosis and AHT
Amplitude of DSSEPs
N13–N20 conduction time
NDI (disability)
At 1-year follow-up:
Control group reverted toward baseline.
Intervention group maintained significant improvements in all measured variables:
Pain (neck and arm)
Disability (NDI)
Cervical lordosis and AHT
DSSEP metrics (latency & amplitude)
N13–N20 conduction time
Conclusions
Adding the Denneroll orthotic device to a standard rehabilitation protocol yielded better and more durable outcomes in structural alignment, pain reduction, function, and nerve conduction in DCR patients.
Improvement in cervical lordosis and reduced forward head posture are likely key drivers of these benefits.
Implications for you when you visit a Chiropractic Biophysics (CBP) practitioner
Supports CBP’s focus on structural rehabilitation of the cervical spine, not just symptom management.
Demonstrates that posture-corrective devices (like Denneroll) enhance long-term therapy outcomes in discogenic radiculopathy.
Highlights importance of combining traction/orthotic correction with multimodal care for sustainable impact.
Provides measurable, objective outcomes (lordosis angle, nerve conduction) that strengthen CBP’s evidence base.
Patient-Friendly FAQ
What is discogenic cervical radiculopathy (DCR)?
A condition where a disc in the neck compresses a nerve root, causing arm pain, numbness, or weakness.
What does ‘hypolordotic cervical spine’ mean?
It means the natural inward curve in your neck is lost or flattened.
What is the Denneroll device?
A posture corrective orthotic placed under the neck to restore the normal cervical curve over time.
Why add it to a rehab program?
It helps restore spinal alignment, which reduces nerve stress and improves function more effectively than rehab alone.
How much improvement did patients see?
At 10 weeks: better spine curve, nerve function, and reduced disability. At 1 year: sustained improvements in all areas.
Do results last?
Yes. The group using the Denneroll maintained gains at 1 year, while rehab-only group regressed.
Who might benefit from this?
Patients with chronic disc-related neck and arm pain who have poor neck curvature and forward head posture.
References:
Moustafa IM, Diab AAM, Harrison DE. Addition of a sagittal cervical posture corrective orthotic device to a multimodal rehabilitation program improves short- and long-term outcomes in patients with discogenic cervical radiculopathy. Arch Phys Med Rehabil. 2016;97(12):2034-2044. doi:10.1016/j.apmr.2016.07.015